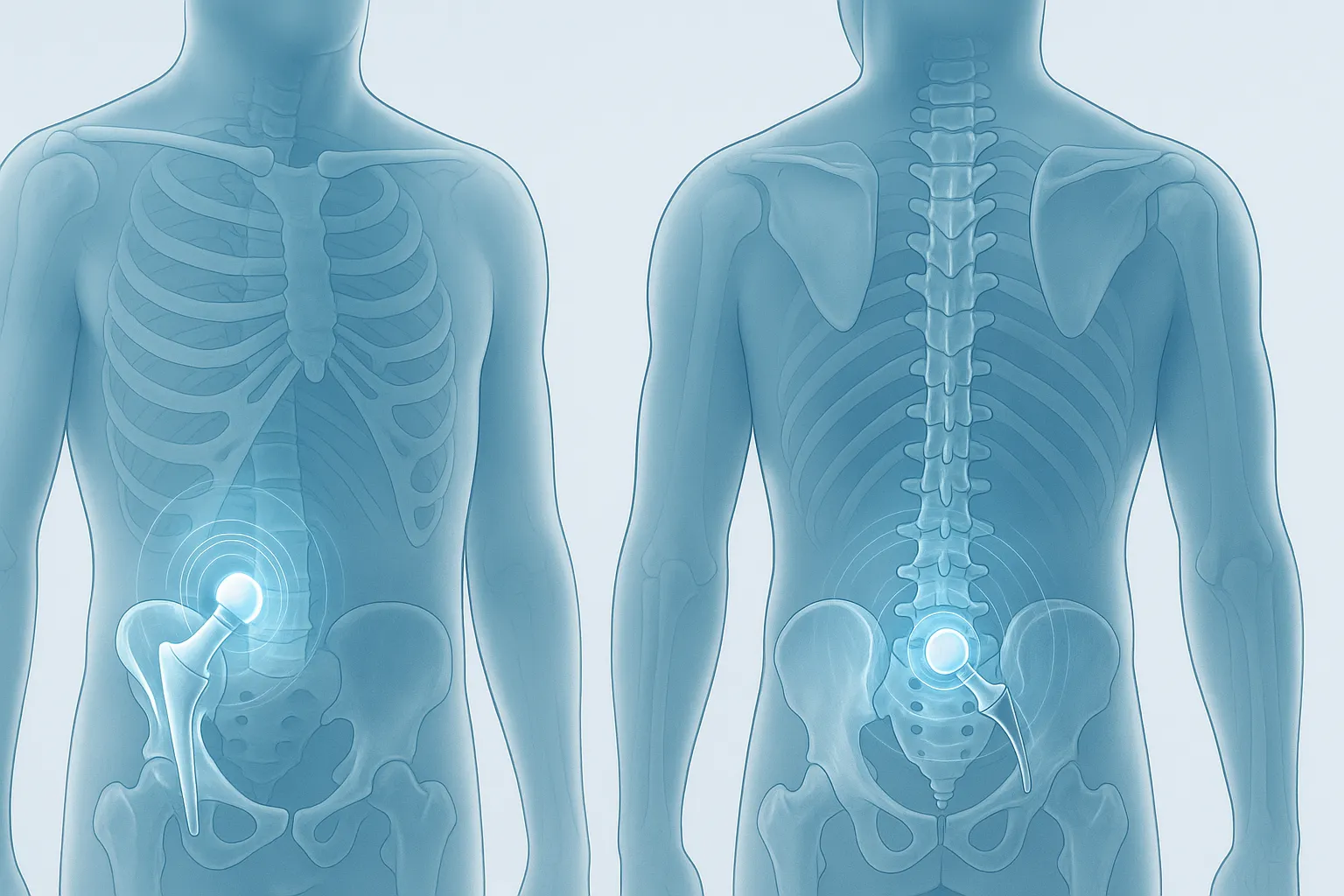
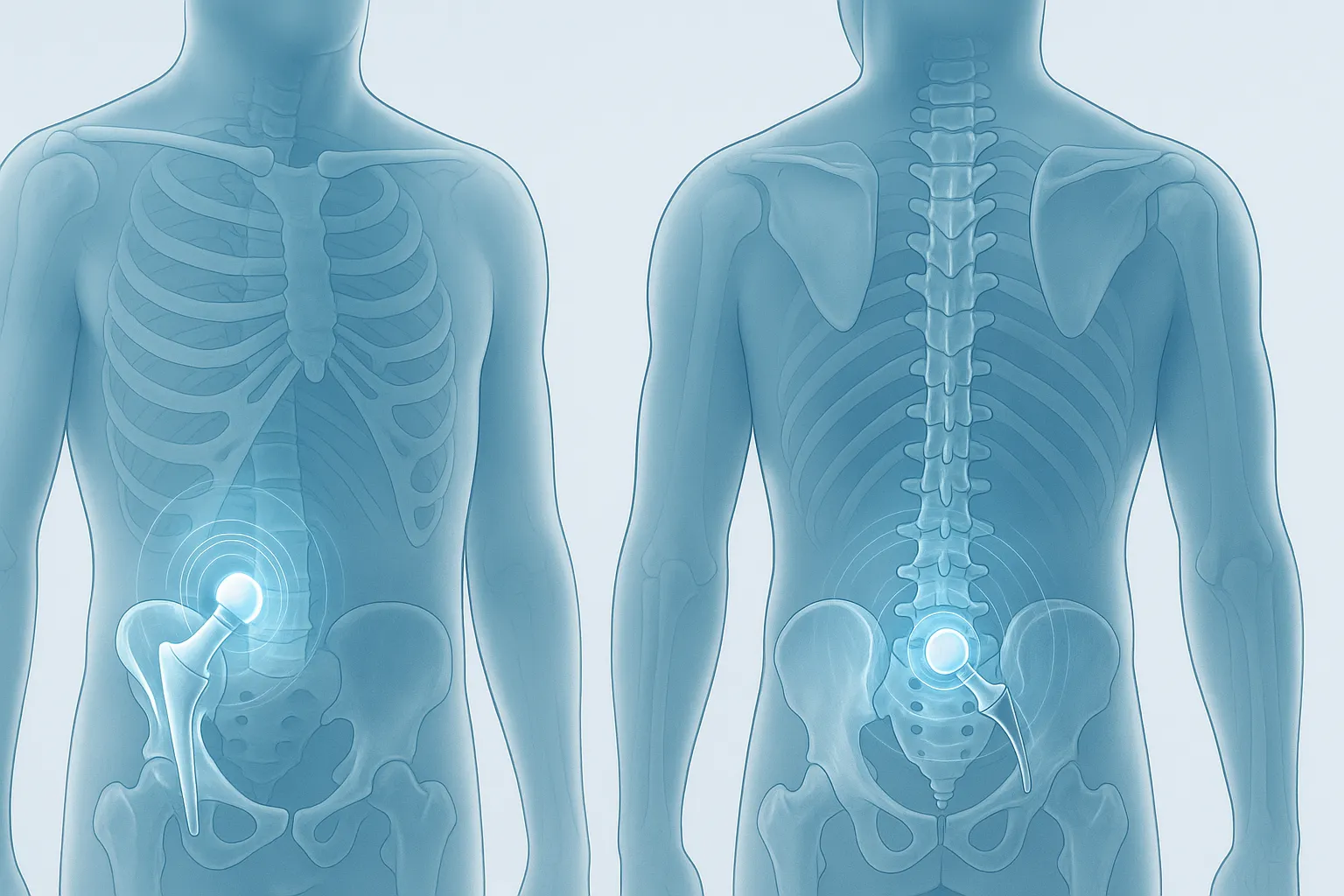
Hip replacement surgery has become one of the most successful procedures in modern orthopaedics, offering reliable pain relief and restoring mobility for people suffering from advanced arthritis, avascular necrosis, trauma-related degeneration, and other debilitating conditions. As surgical techniques evolve, one of the most common questions patients ask is: “Which approach is better — anterior or posterior hip replacement?”
There is no universal “best” approach. Instead, surgeons choose the technique based on the patient’s anatomy, health, mobility goals, and specific pathology. Both approaches aim to replace the worn joint with a prosthetic one, but the way surgeons access the hip differs — and that difference influences the recovery experience, risks, and outcomes.
This article breaks down the anterior and posterior approaches, helping patients better understand what they may expect and how specialists determine the right method for each individual.
Before comparing the two, it helps to understand what the approaches refer to.
They describe the direction and anatomical path the surgeon uses to reach the hip joint.
Both methods successfully replace the hip joint, but access to muscles, soft tissues, and tendons varies — and so do some aspects of recovery.
The anterior approach, also called the “front approach,” has gained attention over recent years for its muscle-sparing nature.
The key takeaway: The anterior approach is muscle-sparing and appealing for recovery-focused patients, but anatomical factors play a big role in eligibility.
The posterior approach has been used for decades and remains one of the most common and trusted methods worldwide.
The key takeaway: The posterior approach remains the gold standard for many cases due to its versatility and excellent long-term outcomes.
Instead of a table, here is a clear list comparing the two approaches using straightforward patient-focused criteria.
Muscle Involvement
Dislocation Risk
Suitability for Complex Cases
Incision Location
Surgeon Experience Factor
Post-Op Restrictions
Body Type Considerations
Operating Room Setup
Long-Term Outcomes
Most studies show no significant difference in long-term pain relief, function, or implant longevity between the two approaches.
In reality, the surgeon’s expertise, experience, and familiarity with the chosen approach often influence outcomes more than the approach itself.
A patient may be a better candidate for one method due to:
The most important step is a personalised conversation with an orthopaedic surgeon who evaluates all variables and guides the patient toward the safest and most effective option.
1. Is the anterior hip replacement less painful?
Many patients report less early pain, but long-term pain relief is similar for both approaches.
2. Does the posterior approach take longer to recover from?
Not always. With modern techniques, recovery differences are minimal after the first few weeks.
3. Is there a difference in long-term outcomes?
No. Both approaches provide excellent long-term results when performed by skilled surgeons.
4. Can I choose which approach I want?
You can express a preference, but your anatomy, medical conditions, and surgeon’s expertise will guide the final recommendation.
5. Are dislocations more common with the posterior approach?
Historically yes, but improved implant designs and soft-tissue repair have dramatically reduced this risk.
6. Why would a surgeon recommend the posterior approach for me?
It offers better access for complex hips, revisions, and patients with higher BMI or unique anatomy.
7. Will I walk sooner with the anterior approach?
Possibly — some patients walk independently earlier, though long-term recovery evens out between approaches.