Knee pain is one of the most common musculoskeletal complaints affecting Australians of all ages. While injuries to ligaments, cartilage, and tendons are widely recognised causes, another increasingly identified contributor is bone marrow lesions (BMLs). These changes are often detected through magnetic resonance imaging (MRI) and can provide valuable insight into joint health, pain severity, and long-term outcomes.
Understanding what bone marrow lesions mean, how they develop, and the available treatment options can help patients make informed decisions about their knee care.
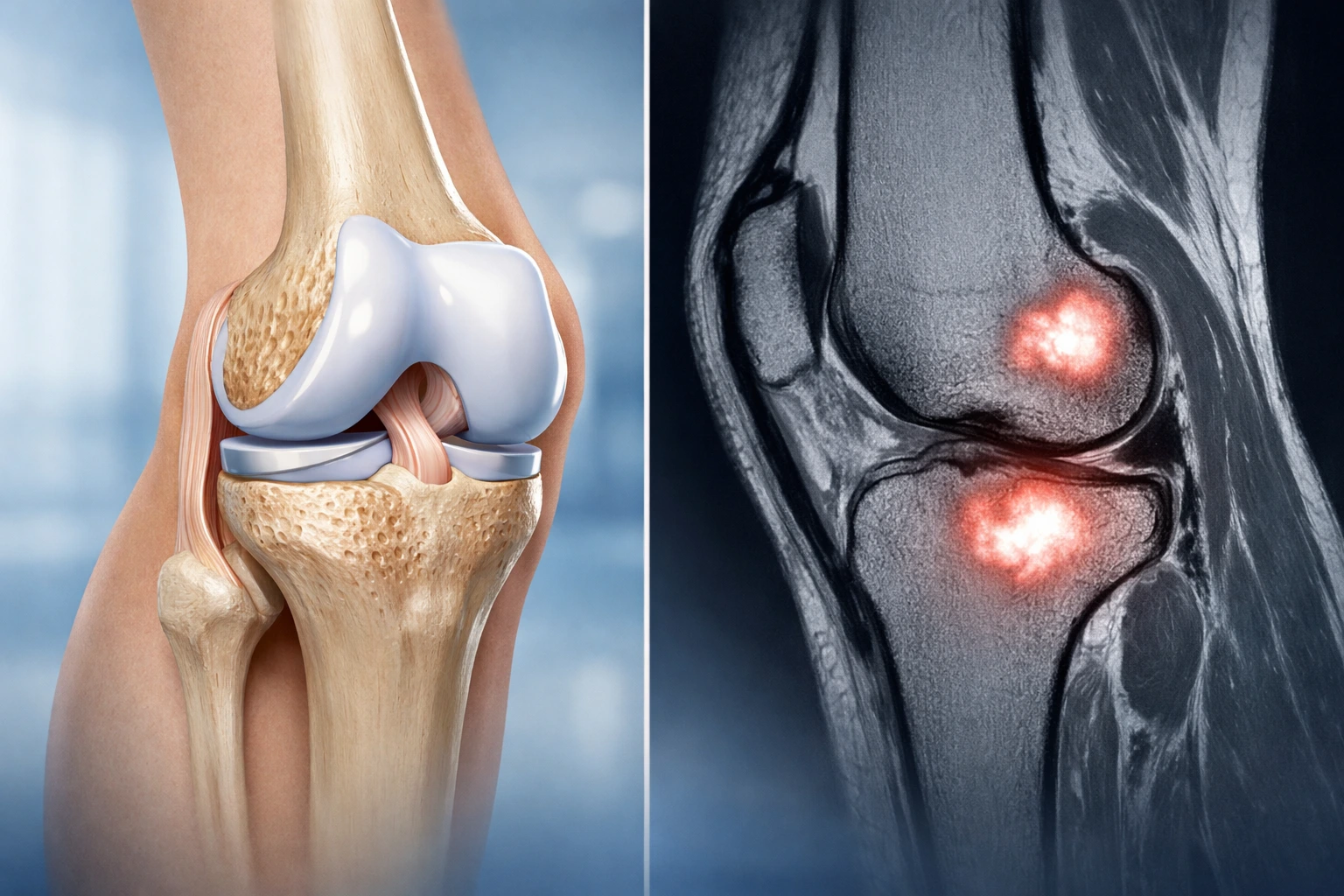
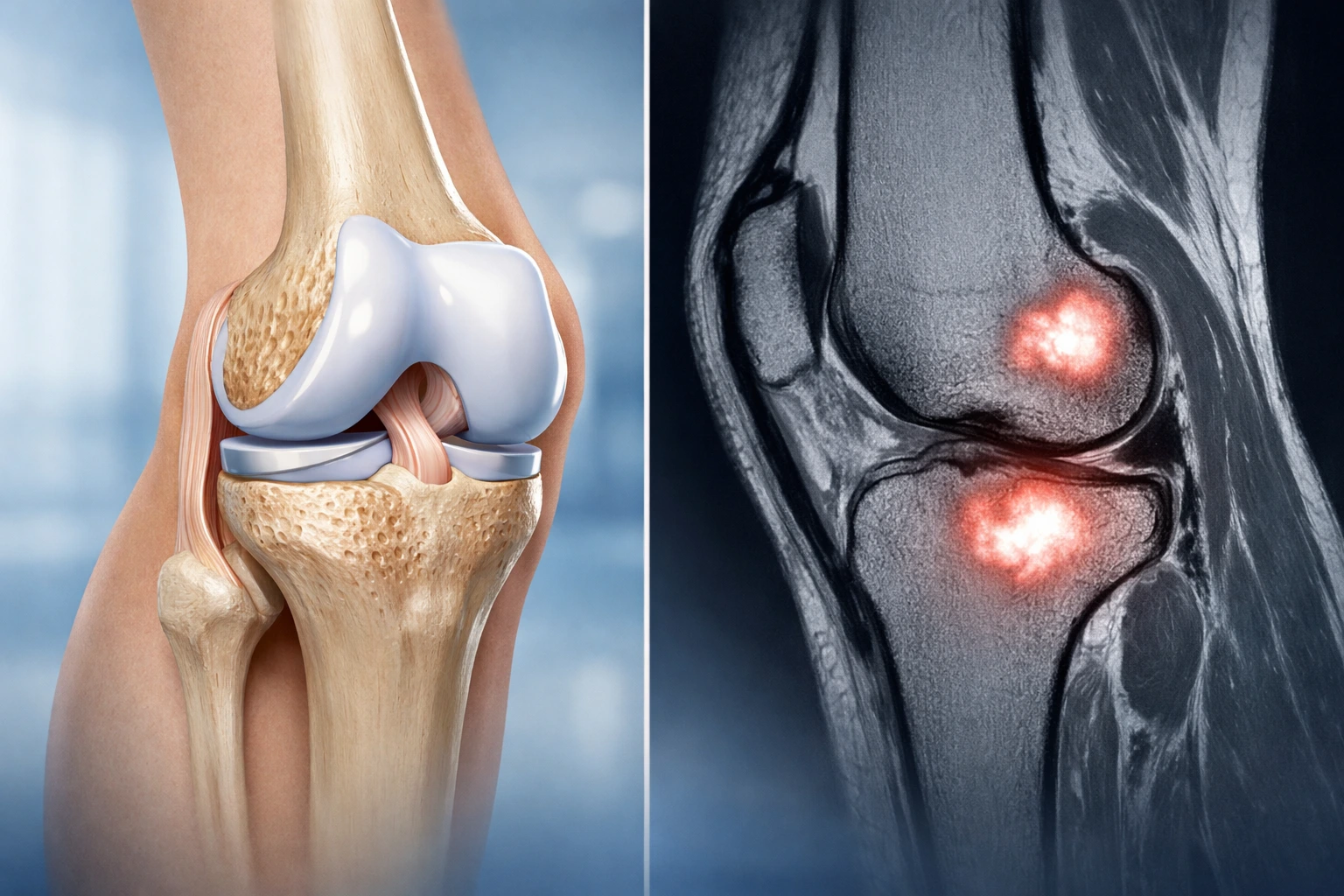
Bone marrow lesions refer to areas within the bone beneath the joint surface that show abnormal changes on MRI scans. These lesions represent regions of increased fluid, inflammation, or micro-damage within the bone marrow.
Although they are sometimes referred to as “bone bruises,” BMLs can involve more complex structural changes. They are most commonly found in the weight-bearing regions of the knee, particularly in patients with osteoarthritis, cartilage damage, or traumatic injuries.
Bone marrow lesions are not always visible on standard X-rays. MRI scans are the most sensitive imaging tool for detecting them, making MRI an important investigation when knee pain persists despite normal X-ray findings.
Bone marrow lesions develop due to excessive stress placed on the joint surface. The knee is particularly vulnerable because it supports body weight and absorbs impact during daily activities such as walking, running, and climbing stairs.
Common causes include:
When cartilage becomes damaged or thins, the bone beneath it absorbs more load. This increased stress can trigger inflammation and structural changes, resulting in bone marrow lesions.
Bone marrow lesions are clinically significant because they are strongly associated with knee pain and disease progression. Studies have shown that patients with BMLs often experience more severe symptoms compared to those without these changes.
Key reasons why BMLs matter include:
While some bone marrow lesions can improve over time, others may persist or enlarge if underlying joint problems are not addressed.
Symptoms can vary depending on the size and location of the lesion as well as the underlying cause. Many patients report symptoms that overlap with other knee conditions.
Common symptoms include:
In some cases, symptoms may develop gradually, while in others they can appear suddenly following injury.
MRI is considered the gold standard for diagnosing bone marrow lesions. It provides detailed images of soft tissues, cartilage, and bone, allowing specialists to identify subtle changes not visible on X-rays or CT scans.
Diagnosis typically involves:
Accurate diagnosis helps guide appropriate treatment planning.
Management of bone marrow lesions depends on several factors including the underlying cause, severity of symptoms, and patient lifestyle. Treatment usually begins with conservative approaches before considering surgical intervention.
Many patients respond well to non-surgical treatment options aimed at reducing joint stress and inflammation while promoting healing.
Common conservative treatments include:
These strategies aim to reduce symptoms and prevent lesion progression.
Some patients may benefit from newer regenerative therapies designed to stimulate tissue repair and reduce inflammation. These may include:
While promising, these treatments are still evolving and may not be suitable for all patients.
Surgery may be recommended when conservative treatments fail to relieve symptoms or when structural joint damage is significant. The choice of surgical procedure depends on the patient’s age, activity level, alignment, and severity of joint degeneration.
Situations where surgery may be considered include:
Depending on the underlying condition, surgical approaches may involve:
A specialist orthopaedic surgeon will assess individual circumstances to determine the most appropriate procedure.
The outlook for patients with bone marrow lesions varies. Smaller lesions associated with acute injuries may resolve over time with appropriate treatment. However, lesions linked to osteoarthritis may persist and require ongoing management.
Early diagnosis and intervention can improve outcomes by reducing pain and slowing joint deterioration. Maintaining knee strength, flexibility, and healthy body weight can also play a crucial role in long-term joint health.
Patients should consider seeking medical assessment if they experience:
Prompt evaluation can help identify underlying problems and prevent further joint damage.
Not exactly. Bone marrow lesions can occur alongside osteoarthritis but are not the same condition. They represent changes within the bone that may contribute to arthritis symptoms and progression.
Some lesions, particularly those caused by injury, can improve with rest and appropriate treatment. Others related to chronic joint stress may persist without targeted management.
Not always. Some patients may have lesions visible on MRI without significant symptoms. However, larger or progressive lesions are more likely to be painful.
Recovery time varies depending on the cause and severity of the lesion. Mild lesions may improve over several months, while more complex cases may require long-term management or surgery.
Yes, but exercise should be guided by a healthcare professional. Strengthening and low-impact activities can support joint stability and reduce symptoms.
No. Many patients improve with conservative treatments. Surgery is typically considered only when symptoms persist or joint damage progresses.
In some cases, particularly when lesions are associated with advanced osteoarthritis, knee replacement may become necessary. Early treatment may delay or prevent this outcome.