The Short Version
- Osteoarthritis (OA) of the knee is the single biggest cause of knee pain in Australia – affecting about 2 million Australians and accounting for one-fifth of the musculoskeletal disease burden.
- Surgery is a last resort. Most people get meaningful relief from a mix of education, exercise therapy, weight management, medicines and targeted injections, guided by updated Australian guidelines issued in 2024.
- Other common non-surgical culprits – such as patellofemoral pain, tendinopathies and meniscal irritation – respond to many of the same conservative strategies, with activity-specific tweaks.
Why Your Knee Hurts: The Australian Picture
Osteoarthritis tops the list. The Australian Institute of Health and Welfare estimates that 8.3 % of the population lives with OA, with the knee the most frequently affected joint. OA now makes up 20 % of the nation’s total musculoskeletal disease burden and shows no sign of slowing as our population ages and BMI rises.
Patellofemoral pain (often labelled “runner’s knee”) is the chief non-arthritic cause, with studies showing an annual prevalence of roughly 23 % in adults.
Traumatic injuries (ligament sprains, meniscal tears) matter too, but for most Australians chronic, load-related problems overshadow acute sport injuries once past their twenties.
The Modern Conservative Toolkit
Current Australian guidance follows a clear hierarchy: start with lifestyle and exercise, layer in pharmacology only as needed, and reserve injections for flares or specific mechanical problems. Here’s what the evidence supports.
1. Education & Self-Management
- Understand the condition. Simple explanations of joint wear, flare triggers and pacing reduce anxiety and improve adherence to exercise.
- Activity modification, not elimination. Swapping high-impact runs for cycling or deep-water running often keeps fitness up while letting inflammation settle.
Why it matters: The 2024 Clinical Care Standard stresses that imaging isn’t needed to start conservative care; informed self-management is.
2. Exercise Therapy – The Undisputed Core
- Quadriceps-strengthening and hip-abductor work cut pain and improve function for OA and patellofemoral pain alike.
- Neuromuscular exercise programmes (e.g. GLAD®) blend strength, balance and movement control and are now available in most Australian capitals.
- Frequency: 2–3 supervised sessions a week for at least 12 weeks; persistence brings the biggest gains.
Every reputable guideline – RACGP, Osteoarthritis Research Society International (OARSI), and Cochrane reviews – lists structured exercise as first-line therapy, independent of age or X-ray severity.
3. Weight Management
For every kilogram lost, knee joint load during daily activities drops by roughly 3 kg. Even a 5 % body-weight reduction can noticeably ease pain. Recent Australian GP journal data confirm that heavier patients gain the largest symptom win per kilo shed.
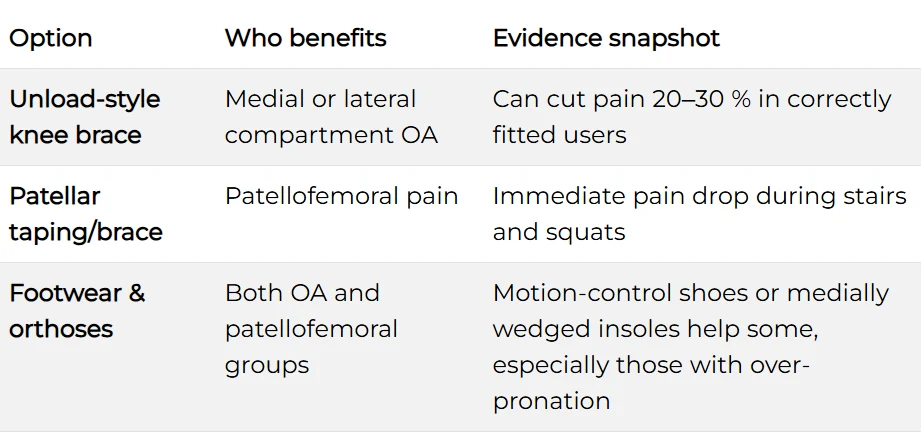
4. Adjunctive Physical Supports

(Use on clinician advice; poor fit can worsen symptoms.)
5. First-Line Medicines
- Topical NSAIDs (e.g. diclofenac gel) – similar pain relief to oral NSAIDs for many, with minimal systemic risk.
- Oral NSAIDs – effective but consider gastro-renal risks; use the lowest effective dose for the shortest time.
- Paracetamol – better than placebo for some, but weaker than NSAIDs; no longer recommended as sole therapy for moderate–severe OA.
Australian practice pearl: Ask your GP about a Chronic Disease Management (CDM) plan; Medicare rebates can subsidise physiotherapy while you trial exercise and topical agents.
6. Targeted Injections

Guidelines place corticosteroid as first-choice for acute inflammatory flare. Viscosupplementation or PRP may be offered when conservative core treatments plateau, but cost and availability vary.
- Other Modalities with Growing Evidence
- Neuromuscular electrical stimulation (NMES) – assists quad activation in severe OA or post-injury atrophy.
- Acupuncture/TENS – modest short-term relief; safe when delivered by registered practitioners.
- Glucosamine & chondroitin – large trials show minimal benefit; discuss cost-benefit before starting.
Putting It Together: A Pragmatic Road-Map
- See your GP for a diagnosis – imaging only if red flags or uncertain findings.
- Begin a structured physio-led exercise programme within two weeks.
- Tackle weight and metabolic health simultaneously; dietitian input helps.
- Layer topical NSAIDs; trial oral NSAIDs if pain limits exercise.
- Add bracing or taping tailored to the specific biomechanical issue.
- Consider an injection for persistent pain flares that block rehab.
- Review progress at 12 and 24 weeks; refine or escalate as needed. Joint replacement should only enter the conversation after well-documented conservative failure and significant quality-of-life loss.
Frequently Asked Questions
Do I really need an MRI?
Usually not. Most degenerative changes visible on MRI do not alter first-line treatment. X-ray alone suffices when imaging is truly required.
Can I keep running?
If pain remains under a 3/10, swelling is absent and gait stays symmetrical, graded running is fine. Otherwise swap in cycle or pool work until symptoms settle.
How long before I feel better?
Most patients report a meaningful improvement within 6–12 weeks of consistent exercise and weight optimisation, though cartilage changes take longer.
Take-Home
Knee pain doesn’t automatically equal surgery. In 2025, Australians have a robust, evidence-backed menu of non-surgical options—anchored in exercise, lifestyle change and judicious medicine use. Start with the basics, stay consistent, and escalate logically with your GP or physiotherapist’s guidance.