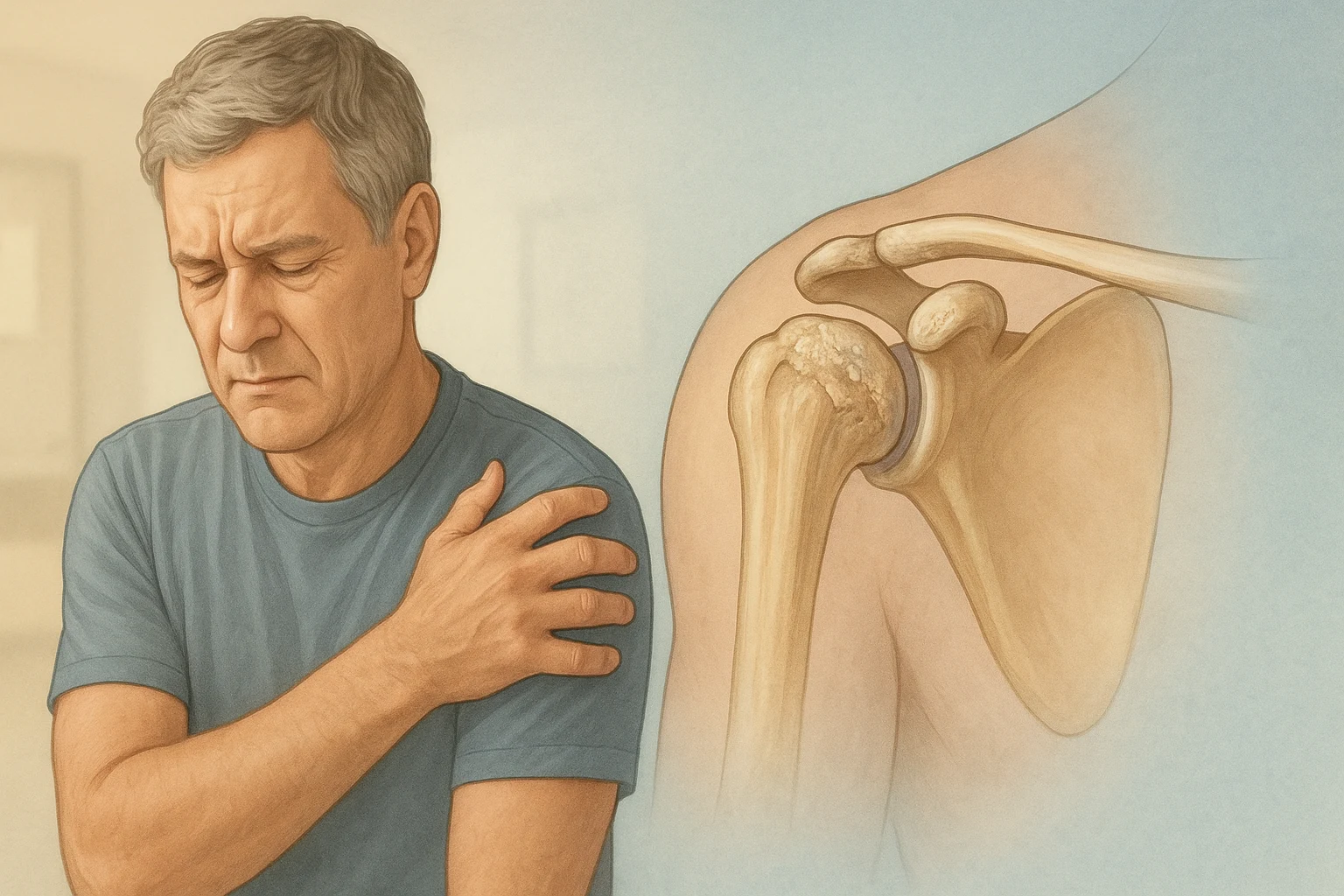
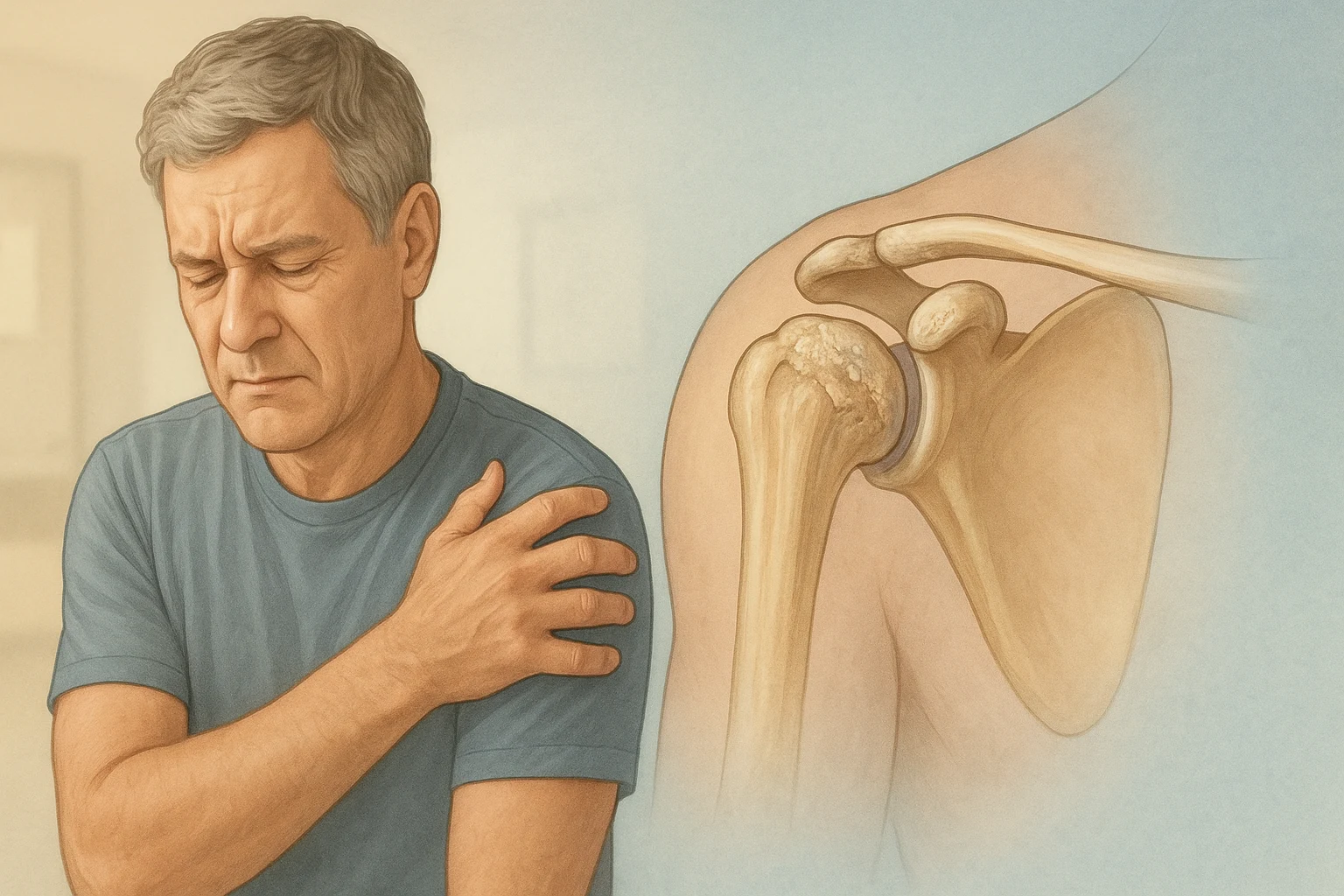
When most people think of arthritis, they picture stiff hips, sore knees, or knobbly finger joints. But the shoulder — our most mobile joint — can be just as vulnerable to wear-and-tear changes. Unfortunately, shoulder arthritis is often missed or misdiagnosed in its early stages, leading to prolonged pain and disability.
One of the main reasons? Shoulder pain can mimic other, more common conditions like bursitis or rotator cuff tendonitis. And while those are treatable with rest, physiotherapy, and injections, arthritis may need a very different approach.
The shoulder joint is a complex ball-and-socket structure surrounded by tendons, ligaments, and bursae (fluid-filled sacs that reduce friction). In arthritis, the smooth cartilage lining the joint wears away, causing bone to rub against bone. This leads to inflammation, stiffness, and reduced range of motion.
Common reasons for misdiagnosis include:
If arthritis isn’t picked up early, patients can spend months — even years — cycling through ineffective treatments. Steroid injections may give only short-term relief, and repeated cortisone use can weaken tendons over time.
In advanced cases, the joint becomes so damaged that pain relief is minimal with conservative options. Everyday tasks like dressing, reaching overhead, or even sleeping comfortably become almost impossible.
For many patients with severe arthritis, especially when the rotator cuff is also damaged, reverse shoulder replacement offers a powerful solution.
How it works:
Reverse shoulder replacement may be considered if:
After surgery, most patients notice pain relief within weeks, with gradual improvement in strength and mobility over several months. A dedicated rehabilitation program is essential, and most people can return to light activities within 6–12 weeks.
Long-term studies show high satisfaction rates, especially in those who had been struggling for years with misdiagnosed or untreated arthritis.
Shoulder arthritis can easily masquerade as other conditions — but an accurate diagnosis is crucial for effective treatment. If your shoulder pain isn’t improving with standard care, it may be worth seeking a specialist opinion and requesting imaging that looks specifically for arthritis.
For those with advanced disease, reverse shoulder replacement can be life-changing, restoring not just shoulder function but overall independence and quality of life.
1. How can I tell if my shoulder pain is arthritis and not tendonitis?
Tendonitis usually causes pain with specific movements or after overuse, and it may settle with rest and physiotherapy. Arthritis pain tends to be deeper, often constant, and is accompanied by stiffness — especially in the morning or after periods of inactivity.
2. Can shoulder arthritis be treated without surgery?
Yes. Early-stage arthritis can often be managed with physiotherapy, activity modification, anti-inflammatory medications, and occasional cortisone injections. However, these treatments may become less effective as the arthritis progresses.
3. What imaging is best for diagnosing shoulder arthritis?
A plain X-ray is usually the first and most useful investigation, as it clearly shows joint space narrowing, bone spurs, and other signs of arthritis. MRI scans are more helpful for assessing rotator cuff tears.
4. How long does a reverse shoulder replacement last?
Modern implants can last 15–20 years or more, depending on factors like activity level, bone quality, and surgical technique.
5. Is reverse shoulder replacement more effective than traditional shoulder replacement?
It depends on the underlying problem. For patients with severe rotator cuff damage and arthritis (known as cuff tear arthropathy), reverse shoulder replacement is often more effective than a traditional replacement.
6. Will I regain full range of motion after surgery?
Most patients regain good functional movement, particularly for daily activities. While the shoulder may not be as mobile as a completely healthy joint, pain relief and improved function are the main benefits.