A shoulder dislocation can be a painful and frightening injury. For many people, the first dislocation occurs during sport, a fall, or an accident and is treated in emergency care with reduction and short-term immobilisation. While some patients recover without further issues, others go on to experience repeated dislocations — often with increasing frequency and less force involved.
Recurrent shoulder dislocations are not simply “bad luck” or weak muscles. They are usually the result of structural instability within the shoulder joint. Without early specialist assessment and appropriate management, repeat dislocations can lead to bone loss, worsening instability, and a significantly higher risk of long-term problems.
This article explains why repeat shoulder dislocations require early specialist care, the role of instability and bone damage, and when surgical stabilisation may be recommended to reduce recurrence risks.
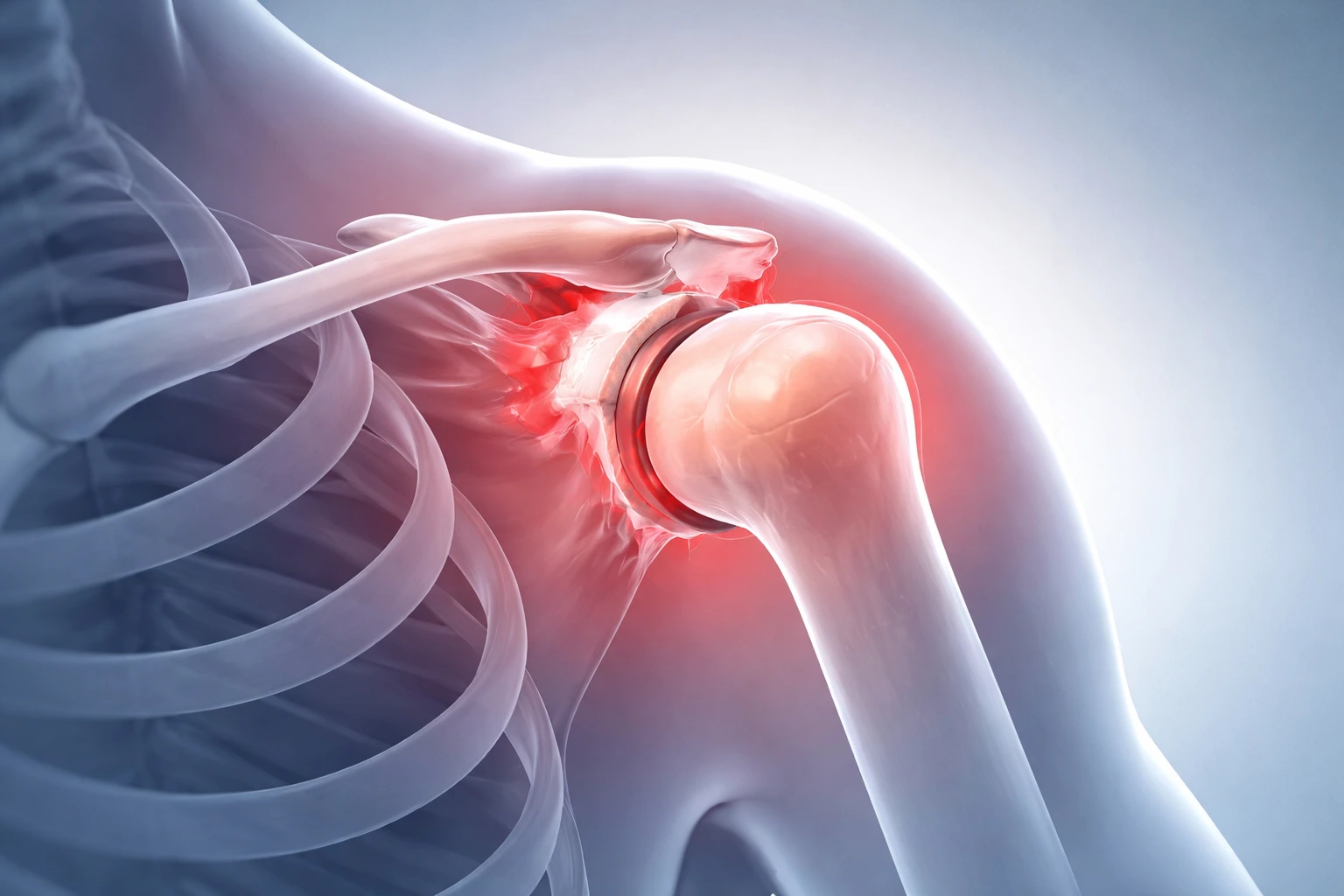
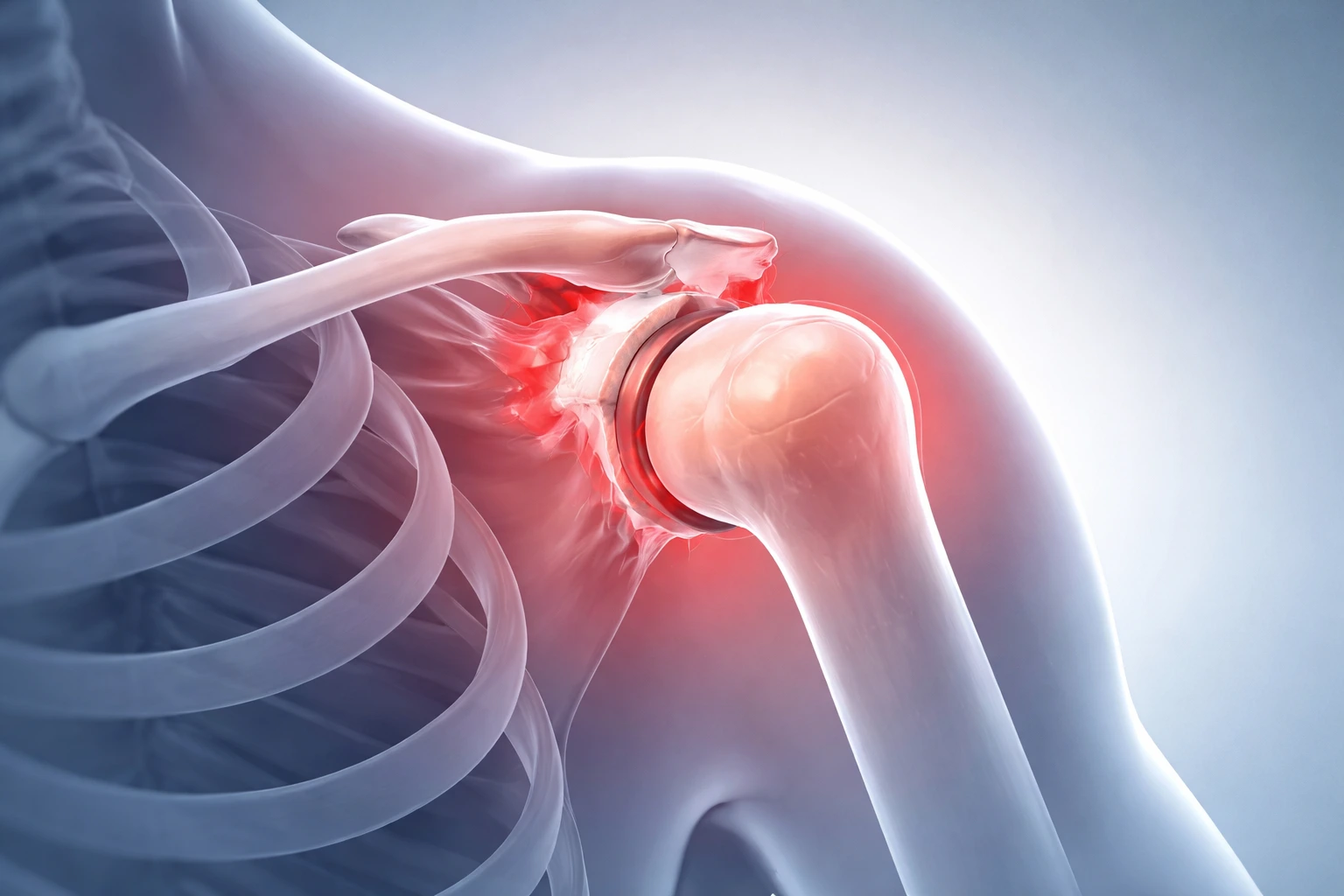
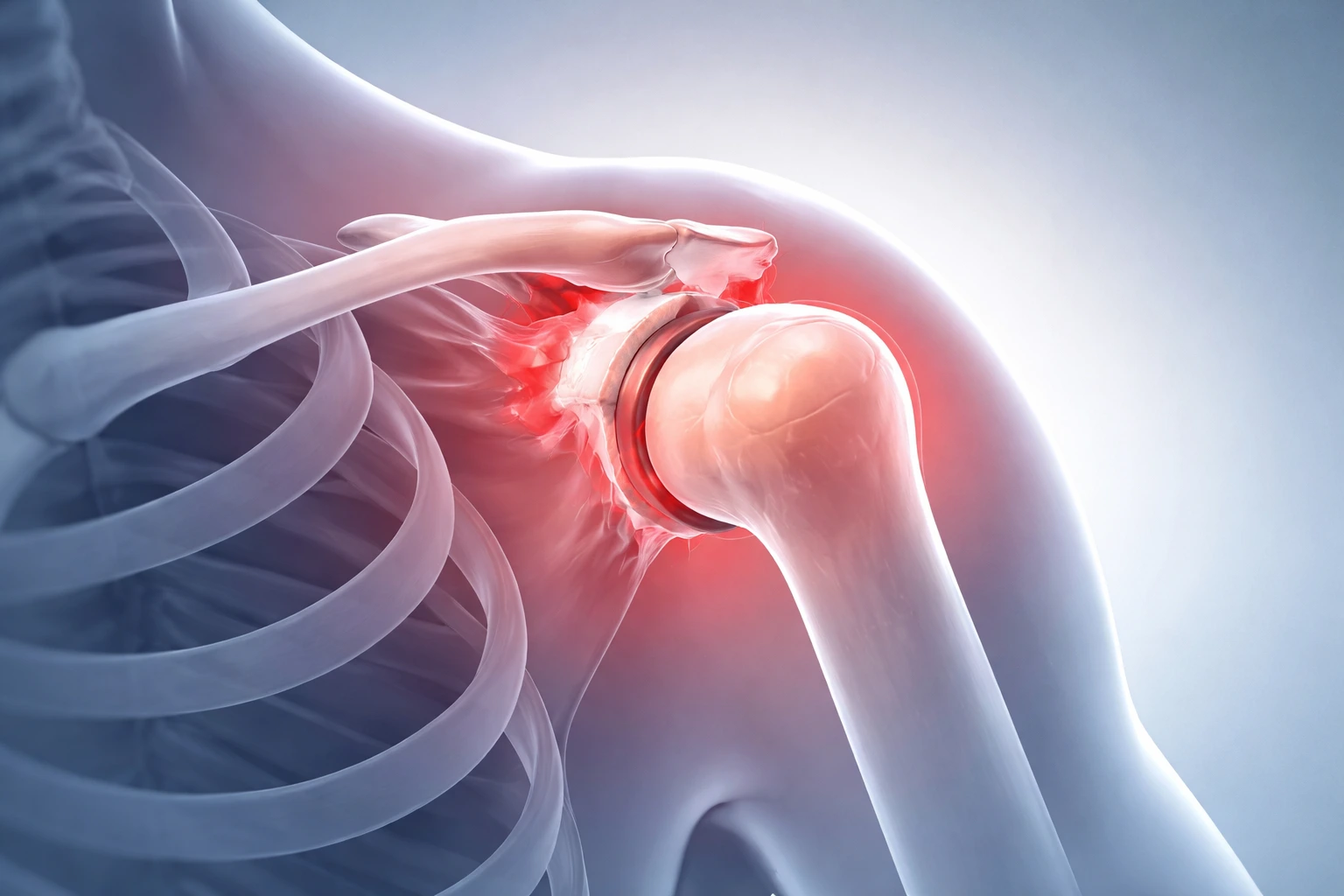
The shoulder is the most mobile joint in the body, allowing a wide range of movement for daily activities and sport. This mobility comes at a cost — the joint relies heavily on soft tissues for stability.
The shoulder joint is stabilised by:
When a shoulder dislocates, these stabilising structures can be damaged. In many first-time dislocations, particularly in younger or athletic patients, the labrum and capsule are torn. This damage may not heal adequately on its own, leaving the shoulder prone to slipping out again.
Once instability develops, the shoulder may dislocate during routine activities such as reaching, lifting, or sleeping — not just during sport or trauma.
Each subsequent dislocation increases the risk of further damage to the shoulder joint. Recurrent dislocations often occur more easily, with less force, and recovery may take longer each time.
Key concerns with repeat shoulder dislocations include:
Importantly, the longer instability is left untreated, the more complex future treatment can become.
One of the most significant risks of repeated shoulder dislocations is bone loss. This can occur on:
Bone loss develops as the joint repeatedly dislocates and impacts against itself. Over time, this changes the shape of the joint and reduces its ability to stay in place.
Why bone loss matters:
In early stages, bone loss may not be obvious on standard X-rays. Specialist assessment and advanced imaging are often required to accurately evaluate the extent of damage.
Some patients are more likely to experience repeat dislocations than others. Factors associated with higher recurrence risk include:
In young, active individuals, recurrence rates after a first dislocation managed without specialist input can be very high. Early referral can significantly reduce the risk of ongoing instability.
While a single dislocation may initially be managed conservatively, early specialist care is strongly recommended if:
A shoulder specialist can assess the degree of instability, evaluate for bone loss, and tailor treatment to your individual risks and goals.
Surgical stabilisation aims to restore stability to the shoulder by repairing or reconstructing damaged structures. The goal is to prevent further dislocations, protect the joint, and allow safe return to activity.
Surgical options may include:
The choice of procedure depends on:
When performed early — before significant bone loss occurs — stabilisation surgery has a higher success rate and may allow a quicker, more reliable recovery.
Delaying specialist care after repeat dislocations can lead to:
Early intervention allows treatment to be tailored before damage becomes severe. In many cases, this can mean less invasive surgery and better long-term outcomes.
Whether managed surgically or non-surgically, rehabilitation plays a crucial role in shoulder stability. A structured program focuses on:
Following specialist guidance during recovery reduces the risk of reinjury and supports long-term shoulder health.
Concept:
A clean, clinical yet dynamic image showing a human shoulder joint in semi-transparent anatomical style. The shoulder is positioned in slight abduction, with subtle highlighting of the joint capsule and labrum. A soft gradient background in neutral blues or greys suggests medical expertise and stability. No text, labels, or logos — the image should visually communicate joint structure, movement, and vulnerability.
A first-time dislocation may settle with rest and rehabilitation, particularly in older or less active individuals. However, if instability persists or the shoulder dislocates again, specialist assessment is important.
More than one dislocation is a warning sign. Recurrent dislocations significantly increase the risk of bone loss and long-term damage.
Not always, but recurrent instability often indicates structural damage. Surgery may be recommended if the risk of recurrence is high or if bone loss is present.
Ongoing instability can lead to worsening bone damage, reduced shoulder function, and a higher likelihood of arthritis later in life.
Recovery varies, but most patients return to daily activities within weeks and sport or heavy work within several months, following structured rehabilitation.
Yes. Many patients return to sport successfully, particularly when surgery is performed early and rehabilitation is followed carefully.