Understanding Shoulder Osteoarthritis: What It Means & What to Do
Summary
Shoulder osteoarthritis is often overlooked compared to hip or knee arthritis, but it can significantly affect mobility, sleep, and daily function. This article explores what shoulder osteoarthritis is, who’s at risk, how it affects the joint, and practical steps for early management—including both surgical and non-surgical options.
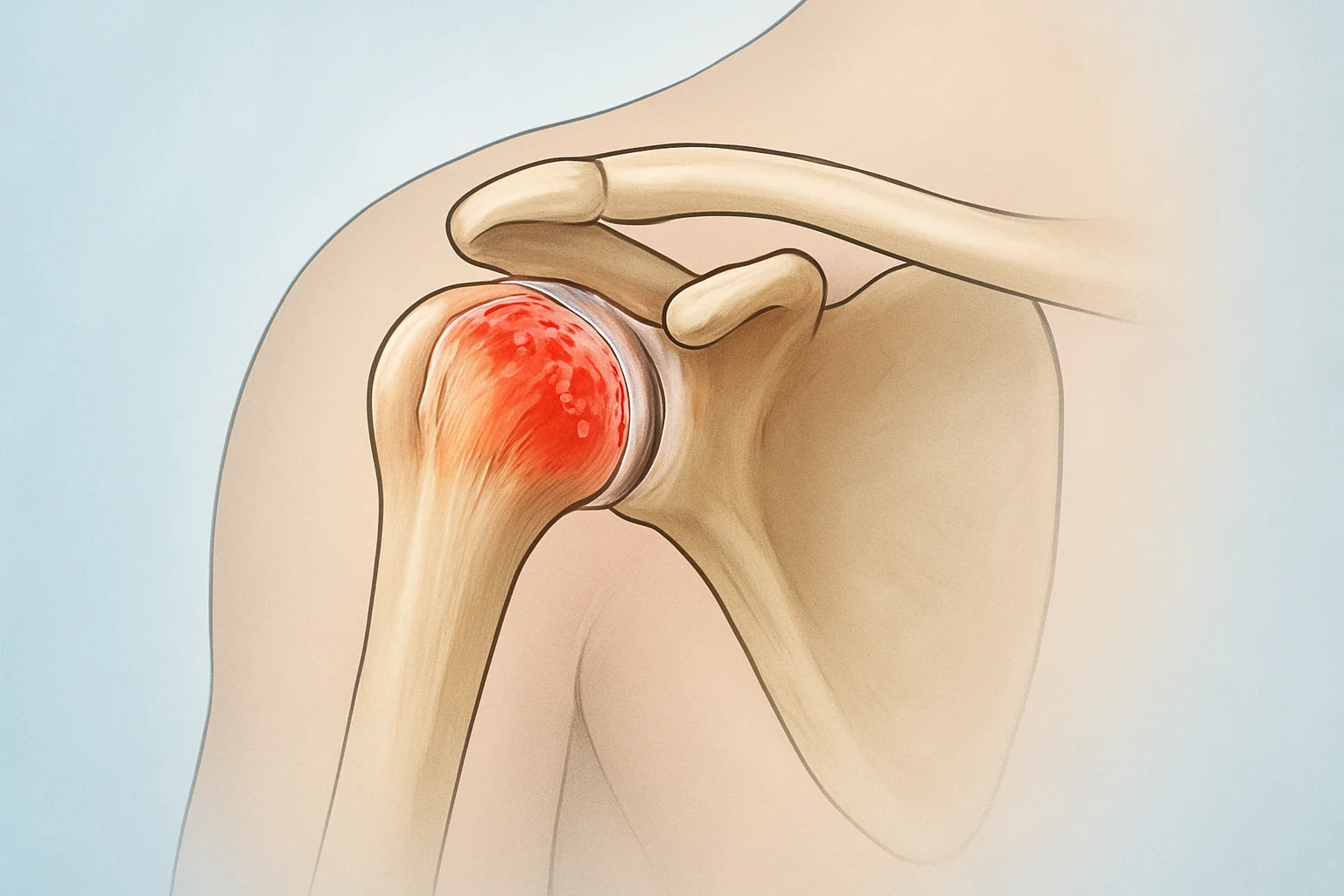
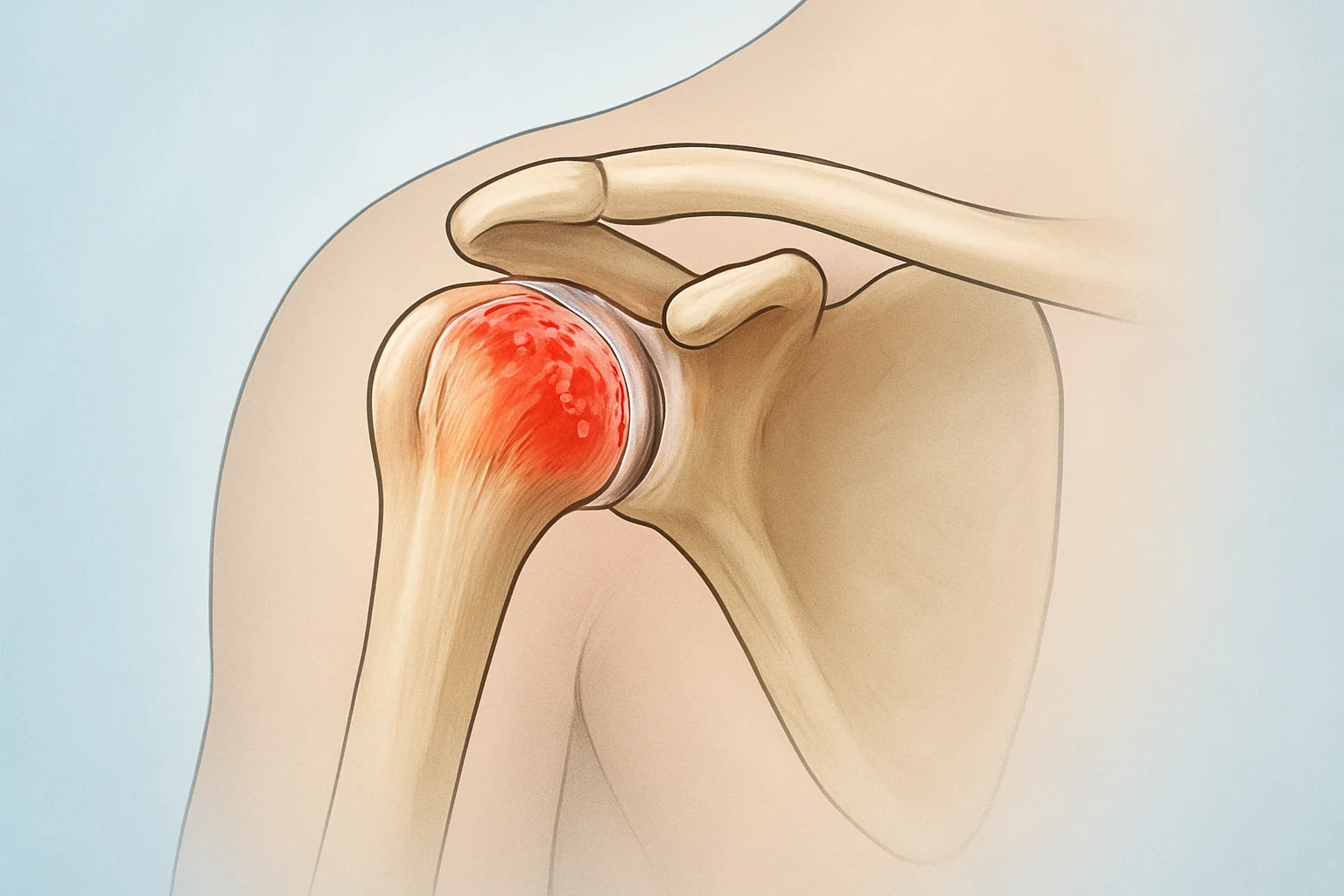
What Is Shoulder Osteoarthritis?
Shoulder osteoarthritis (OA) occurs when the cartilage that cushions the bones in the glenohumeral (shoulder) joint gradually wears away. Over time, this leads to friction between bones, causing pain, stiffness, and reduced range of motion.
Most people associate osteoarthritis with the hips or knees. However, the shoulder is the third most common joint to develop osteoarthritis in older adults. It affects both active and sedentary individuals, especially those with a history of repetitive shoulder use or injury.
Who Is at Risk of Shoulder Osteoarthritis?
- Ageing adults – especially those over 50
- Athletes or manual workers – repetitive overhead use increases wear
- Previous shoulder injury – fractures, dislocations, or rotator cuff damage
- Genetic predisposition
- Inflammatory joint disease
Common Symptoms of Shoulder Osteoarthritis
Shoulder OA tends to progress slowly, making symptoms easy to overlook until they significantly impact function. Common signs include:
- Deep, aching pain – especially when lifting or rotating the arm
- Reduced range of motion – trouble reaching high shelves or fastening a bra/shirt
- Grinding or clicking sensations – from bone friction
- Swelling and stiffness – especially in the morning or after inactivity
- Night pain – difficulty sleeping on the affected shoulder
If you're experiencing any of these symptoms, consulting an orthopaedic specialist early can slow progression and preserve function.
Causes of Shoulder Osteoarthritis
Shoulder cartilage wears down gradually, but several factors can speed up the process:
- Age and joint degeneration
- Trauma or repetitive use
- Inflammatory conditions like rheumatoid arthritis
- Genetics
- Occupational or sporting stressors (e.g., painters, swimmers)
Understanding the cause helps shape the most effective treatment plan.
How Is Shoulder Osteoarthritis Diagnosed?
Your orthopaedic surgeon or healthcare provider may use the following tools:
- Medical history & physical exam
- X-ray – reveals bone spurs or decreased joint space
- MRI – examines soft tissues like cartilage and rotator cuff
- CT scan – provides detailed bone structure
Non-Surgical Management Options
Shoulder osteoarthritis can often be well managed without surgery, especially in the early stages. Key approaches include:
- Lifestyle adjustments – avoid repetitive overhead movement, modify physical activity
- Physiotherapy – improve mobility and strengthen surrounding muscles
- Medications – pain relievers, anti-inflammatories
- Joint injections – such as corticosteroids or regenerative injections
- Heat therapy – to relieve stiffness and increase blood flow
- Home exercise programs – daily stretching and strengthening
These interventions aim to reduce pain, improve function, and delay the need for surgery.
When Surgery Becomes an Option
If conservative treatments no longer help and pain affects daily life, surgical options may be considered. They include:
- Arthroscopic debridement – cleaning out debris in mild-to-moderate cases
- Partial shoulder replacement (hemiarthroplasty) – replacing only the humeral head
- Total shoulder replacement – replacing both sides of the joint for severe OA
- Reverse shoulder replacement – for cases involving rotator cuff damage
Your surgeon will determine the best option based on age, activity level, and joint condition.
Daily Living Tips for Managing Shoulder Osteoarthritis
- Sleep with extra pillows for support or consider a back-sleeping position
- Use heat packs in the morning and ice after activity
- Prioritise low-impact exercises, such as walking or swimming
- Work with a physiotherapist for structured movement
- Avoid sudden, repetitive overhead lifting
Frequently Asked Questions (FAQ)
Is shoulder osteoarthritis permanent?
Yes, osteoarthritis is a degenerative condition. While it can’t be reversed, early management can slow progression and reduce pain.
Can physiotherapy help with shoulder arthritis?
Absolutely. Physiotherapy improves range of motion, reduces pain through targeted exercises, and helps strengthen muscles that support the joint.
Will injections cure shoulder osteoarthritis?
No—while injections won’t “cure” arthritis, they can reduce inflammation and pain for several months.
How long does a shoulder replacement last?
Shoulder replacements can last 10–20 years depending on activity level, implant type, and overall health.
What’s the difference between shoulder osteoarthritis and rotator cuff tear?
- Osteoarthritis affects the joint cartilage and bone, while a rotator cuff tear involves damage to the tendons surrounding the shoulder joint. Both can occur together in severe cases.