What is the success rate?
Reverse shoulder replacement surgery has a high success rate in appropriately selected patients. Most studies report that over 90 per cent of patients experience significant pain relief and improved shoulder function following surgery. The procedure is particularly effective for people with severe arthritis combined with an irreparable rotator cuff tear, where conventional shoulder replacement would not be suitable. Success is measured not only by pain reduction but also by improvements in daily activities such as reaching overhead, dressing, and personal care. In Australia, outcomes are closely monitored through orthopaedic registries, and the data consistently show strong patient satisfaction rates. The key to success lies in careful patient selection, precise surgical technique, and adherence to a well-structured rehabilitation program. While the majority of patients achieve excellent results, factors such as age, bone quality, and general health can influence outcomes. As with any major surgery, there is always a small risk of complications that can affect the result. However, when performed by experienced orthopaedic surgeons using modern prosthetic designs, reverse shoulder replacement remains one of the most reliable options for restoring shoulder function and quality of life in patients with complex shoulder conditions.
How long will it last?
A reverse shoulder replacement is designed to be long-lasting, with most implants functioning well for 15 to 20 years or more. Advances in implant design, materials, and surgical techniques have significantly improved durability. The components are typically made of high-grade metal alloys and polyethylene, designed to withstand years of movement and load. The longevity of the prosthesis depends on several factors, including patient activity level, bone quality, surgical precision, and adherence to post-operative guidelines. Younger or more active individuals may experience greater wear over time, while older or lower-demand patients often enjoy longer implant survival. In Australia, registry data from the Australian Orthopaedic Association National Joint Replacement Registry shows consistently good long-term outcomes for reverse shoulder arthroplasty. Regular follow-up appointments and periodic X-rays allow early detection of any loosening or wear. If the shoulder remains pain-free and functional, no further intervention is usually required. With appropriate care, most patients can expect many years of reliable use, often outlasting the lifespan of traditional shoulder replacements in similar clinical situations.
What is the recovery like?
Recovery from reverse shoulder replacement occurs in several stages. Immediately after surgery, patients typically stay in hospital for one to two days. The arm is placed in a sling to protect the joint and support healing. Pain is managed through medication and sometimes a nerve block. Physiotherapy begins early, often within the first day or two, focusing initially on gentle movements of the hand, wrist, and elbow to maintain circulation. Over the next few weeks, guided exercises help restore controlled movement of the shoulder while avoiding strain on the healing tissues. Around six weeks after surgery, the sling is gradually phased out, and more active range-of-motion exercises begin. Strengthening exercises, particularly for the deltoid muscle, are introduced as healing progresses. Most patients can resume light daily activities within six to eight weeks and experience continued improvement for up to a year. Recovery requires patience and consistent physiotherapy, as the shoulder learns to function differently due to the reversed joint mechanics. Success relies on following medical advice, avoiding heavy lifting early on, and attending scheduled follow-up appointments to monitor progress.
Will I need a second surgery?
While most patients enjoy long-term success after reverse shoulder replacement, a small number may eventually require revision surgery. This can occur if the implant wears out, loosens, becomes infected, or if bone quality around the implant deteriorates. Registry data suggests that less than 5 per cent of patients need revision surgery within the first ten years. Advances in implant materials and design have significantly reduced failure rates. The likelihood of needing another operation depends on several factors, including patient age, activity level, bone quality, and adherence to post-operative care. Younger or more active patients are more likely to place higher demands on the joint, potentially leading to earlier wear. However, most older adults who undergo this procedure can expect their implant to last the rest of their lifetime. Regular follow-up appointments help detect any issues early, allowing for intervention before serious complications occur. If revision is required, modern techniques and improved prosthesis designs provide excellent options for maintaining shoulder function and comfort.
How is this different from traditional replacement?
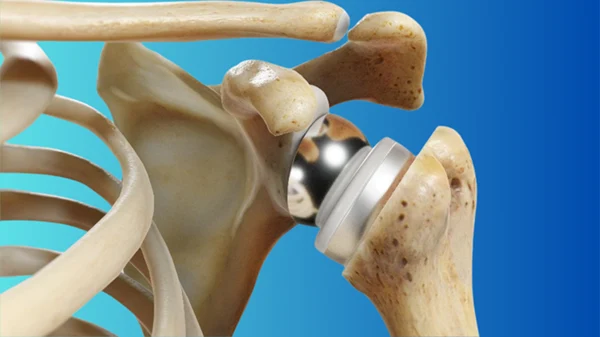
The main difference between reverse shoulder replacement and a traditional (anatomical) shoulder replacement lies in how the joint mechanics are re-engineered. In a conventional replacement, the ball is attached to the humerus (upper arm bone) and the socket to the shoulder blade. This relies heavily on the rotator cuff tendons to move and stabilise the shoulder. In contrast, a reverse shoulder replacement switches the ball and socket positions: the ball component is placed on the shoulder blade, and the socket is attached to the humerus. This change allows the larger deltoid muscle to compensate for a deficient rotator cuff, enabling the arm to lift and function more effectively. The reverse design is particularly beneficial for patients with massive, irreparable rotator cuff tears or arthritis known as cuff tear arthropathy. It is also used in cases of failed previous replacements or complex fractures. The surgery’s biomechanics provide stability and strength where the rotator cuff can no longer do so. Recovery and rehabilitation are similar but tailored to the altered mechanics. The reverse design has proven to deliver excellent outcomes in appropriately selected patients.
What is the recovery time?
Recovery time following reverse shoulder replacement varies depending on the patient’s overall health, pre-operative condition, and adherence to rehabilitation. Most patients spend one to two nights in hospital and wear a sling for four to six weeks. During this time, physiotherapy focuses on gentle, passive movements to protect the repair. After six weeks, guided active exercises begin to improve range of motion, followed by strengthening from about three months. Most patients regain comfortable shoulder movement for daily activities by three to four months post-operation, though complete recovery and maximum improvement in strength can take up to 12 months. Driving and light activities often resume after six to eight weeks, depending on pain and function. It is important to understand that recovery does not mean simply healing from surgery; it involves retraining muscles and adapting to the new joint mechanics. Patience and commitment to physiotherapy are key to achieving the best possible outcome. The recovery process may be slower in patients with pre-existing shoulder stiffness or multiple prior surgeries but remains highly rewarding in most cases.
Will I regain full strength?
After reverse shoulder replacement, most patients regain a substantial amount of functional strength, though not necessarily full pre-injury strength. Because the surgery alters shoulder mechanics, the deltoid muscle takes over much of the lifting work that the rotator cuff once did. As this muscle strengthens through physiotherapy, patients generally experience marked improvements in the ability to raise the arm, reach overhead, and perform daily tasks. While heavy lifting or high-impact sports may remain limited, the regained function is usually more than sufficient for independent living and moderate physical activity. Studies show that the majority of patients can achieve shoulder strength adequate for household activities, gardening, and recreational pursuits such as swimming or golf. Full recovery of strength depends on pre-existing muscle condition, commitment to rehabilitation, and the absence of complications. Those with severe rotator cuff deficiency may notice some limitation in rotational strength but benefit greatly in forward and overhead motion. The primary goal of this procedure is pain relief and restored function rather than complete restoration of athletic power, and in this regard, success rates remain very high.
What are the risks?
As with any major joint replacement, reverse shoulder replacement carries certain risks, although serious complications are relatively uncommon. Potential risks include infection, nerve injury, fracture, instability, and loosening of the implant over time. Infection is one of the most significant concerns, occurring in a small percentage of patients. It can require antibiotics or, in rare cases, further surgery. Other complications include shoulder dislocation, particularly if post-operative restrictions are not followed, or fracture of the humerus or scapula during or after surgery. Some patients may experience stiffness, reduced range of motion, or persistent discomfort, though these are less common when physiotherapy is followed diligently. Anaesthetic risks, such as allergic reactions or heart-related events, are also possible but generally low with modern monitoring. Long-term risks include wear of the implant components and potential loosening, which might eventually require revision surgery. Comprehensive pre-operative planning, meticulous surgical technique, and adherence to rehabilitation guidelines significantly minimise these risks. Discussing individual risk factors with the surgeon before surgery helps ensure realistic expectations and a smoother recovery journey.
How long will the new joint last?
Modern reverse shoulder replacements are built to be durable, with most lasting 15 to 20 years or more. Advances in materials such as highly cross-linked polyethylene and improved fixation methods have greatly extended implant lifespan. Long-term data from Australian and international joint registries indicate high implant survival rates, with only a small proportion requiring revision within ten years. Longevity depends on factors such as patient age, activity level, surgical precision, and bone quality. Patients who maintain a moderate activity level, avoid repetitive heavy lifting, and attend routine follow-up appointments can expect the implant to last well beyond a decade. As with any mechanical device, wear may occur over time, leading to potential loosening or reduced motion. However, for most patients, especially those over 65, the replacement is likely to last for the remainder of their life. Regular check-ups and imaging can detect any issues early, allowing intervention before significant problems develop. Overall, reverse shoulder replacement remains one of the most durable and effective reconstructive options for severe shoulder dysfunction.