How long will the repair last?
The longevity of a Bankart repair depends on both surgical precision and patient behaviour after the operation. When performed correctly and followed by appropriate rehabilitation, the results are typically long-lasting, providing shoulder stability for many years, often for life. Studies report that the majority of patients maintain stability for more than a decade after surgery. However, durability can be influenced by age, level of physical activity, and whether the shoulder sustains further trauma. Younger, highly active patients—especially those engaged in contact or overhead sports—have a slightly higher risk of recurrence. Once the repaired labrum and capsule fully heal, the shoulder functions normally, but it is still important to maintain muscle strength and joint flexibility to protect against future injury. Avoiding high-risk activities too early after surgery and completing the rehabilitation program are essential for long-term success. For most patients, a Bankart repair offers a permanent solution to recurrent shoulder dislocations, allowing them to return to daily activities and sports with confidence and without instability.
What is the recovery like?
Recovery from Bankart repair surgery is gradual and requires commitment to physiotherapy and adherence to restrictions during the early phase of healing. Initially, the shoulder is immobilised in a sling for about four to six weeks to allow the repaired tissue to heal. During this time, patients focus on pain control, maintaining elbow and wrist movement, and preventing stiffness in the hand and fingers. Once the surgeon and physiotherapist determine it is safe, passive range of motion exercises begin to gently restore flexibility without straining the repair. Around six to twelve weeks after surgery, active exercises are introduced to rebuild shoulder muscle strength and control. Full recovery, including return to sports and heavy activities, typically occurs between four and six months, although this may vary depending on the individual’s healing, the type of work or sport they perform, and their overall fitness. Many patients describe the recovery as a steady process that requires patience and consistency. Pain and stiffness are common early on but gradually subside. Physiotherapy is a critical component, guiding each stage to avoid overloading the repair while promoting optimal shoulder function. By twelve months, most patients achieve excellent stability and confidence in their shoulder.
Will I regain full range of motion?
After a Bankart repair, most patients regain near-normal or full range of motion, though this can vary slightly depending on the extent of the initial injury, the surgical technique used, and the individual’s dedication to rehabilitation. Early after surgery, motion is deliberately restricted to protect the healing tissues. Over time, the physiotherapist introduces progressive exercises that focus on flexibility, strength, and control. Typically, by three to six months, patients regain most of their range, and by twelve months, many achieve their pre-injury level of movement. However, a small degree of stiffness or tightness, particularly in external rotation, is not uncommon. This is often intentional, as the surgery tightens the joint capsule to improve stability and prevent further dislocations. For most daily activities, this minor restriction does not cause functional problems. Athletes or individuals involved in overhead or throwing sports may need longer rehabilitation to restore the fine balance between mobility and stability. Long-term studies show that with proper rehabilitation and adherence to physiotherapy, over 90% of patients regain a functional and pain-free range of motion sufficient for normal life and recreational sport. Early and safe progression guided by a shoulder specialist physiotherapist is vital for optimal recovery.
Will I need a second surgery?
In most cases, a second surgery is not required after a Bankart repair, provided the shoulder heals well and no new trauma occurs. Success rates are high, with 85–95% of patients achieving lasting shoulder stability. However, in a small proportion of individuals, particularly those engaged in high-contact or overhead sports, re-dislocation or recurrent instability may occur. This can happen if the repaired tissue stretches or re-tears, or if there is underlying bone loss that was not addressed during the first procedure. If instability recurs, revision surgery might be needed. In such cases, the surgeon may consider a repeat arthroscopic repair or an alternative stabilisation procedure such as a Latarjet operation, especially if there is significant bone deficiency. The likelihood of needing a second operation is influenced by patient age, activity level, surgical technique, and commitment to rehabilitation. Younger patients, particularly those under 20, are more prone to recurrence. To minimise the risk of needing further surgery, patients should follow post-operative restrictions carefully, complete their physiotherapy program, and avoid premature return to sport. When properly managed, most patients retain stable shoulders long-term and never require another operation.
How long does surgery last?
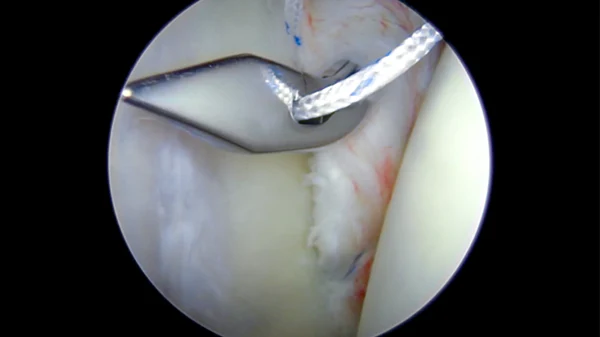
A typical arthroscopic Bankart repair takes about one to one and a half hours to complete, although the duration can vary depending on the complexity of the injury, the presence of associated damage, and the surgeon’s technique. During the operation, the patient is usually placed under general anaesthesia, sometimes combined with a regional nerve block for post-operative pain relief. Once the shoulder is prepared and sterile drapes are in place, the surgeon inserts a small camera (arthroscope) into the joint through a keyhole incision to visualise the torn labrum and capsule. Additional small incisions are used to insert instruments and anchors to reattach the labrum to the glenoid rim. If the injury is more complex or there are additional tears, such as a SLAP lesion or cartilage damage, the operation may take longer. Open procedures, though less common, can extend beyond two hours. After the repair, sterile dressings are applied and the shoulder is placed in a sling. While the surgery itself is relatively short, patients should expect to spend several hours in the hospital for pre-operative preparation and post-operative recovery monitoring before discharge. Most procedures are performed as day surgery.
What is the recovery process?
The recovery process after a Bankart repair follows a structured, phased approach focused on protecting the repair, restoring motion, and gradually rebuilding strength. In the first phase, which lasts about four to six weeks, the shoulder remains in a sling to allow soft tissue healing. Gentle pendulum exercises and hand, wrist, and elbow movements are encouraged to prevent stiffness. During the second phase, from six to twelve weeks, passive and assisted range of motion exercises begin under physiotherapist supervision. The aim is to restore movement without compromising stability. In the third phase, starting around three months, strengthening exercises are introduced to improve control and function of the shoulder muscles, particularly the rotator cuff and scapular stabilisers. The final phase involves sport- or work-specific training, with gradual return to overhead or contact activities between four and six months, depending on progress and surgeon approval. Pain and swelling decrease steadily, though fatigue and mild stiffness can persist for several months. Commitment to physiotherapy and avoiding early overuse are crucial to achieving the best outcomes. Full recovery, including confidence in shoulder stability and performance, typically occurs between six and twelve months.
Will I regain full range of motion?
Most patients regain near-full range of motion after a Bankart repair, although the timeline and degree of recovery vary among individuals. Initially, range of motion is restricted to protect the healing labrum and capsule. As rehabilitation progresses, movement is gradually increased under physiotherapy supervision. By three months, patients usually achieve good mobility, and by six months, many return to their normal level of activity. A small percentage of patients may experience minor limitations in external rotation, which can be a result of the tightened capsule providing additional stability. This restriction is often intentional and does not interfere with most daily or athletic activities. Complete recovery depends heavily on adherence to rehabilitation and avoiding premature stress on the repair. Patients who follow a structured physiotherapy plan are more likely to regain full, pain-free movement. Overstretching or skipping rehabilitation steps, however, can delay or compromise results. With proper care, the majority of patients achieve functional and symmetrical motion compared to the unaffected shoulder, allowing them to resume normal activities, exercise, and even return to sport.
What are the risks?
As with all surgical procedures, Bankart repair carries certain risks, although serious complications are uncommon. The most significant risks include infection, bleeding, nerve or blood vessel injury, stiffness, and failure of the repair leading to recurrent instability. Some patients may experience numbness around the shoulder or mild weakness, which usually resolves over time. Stiffness or restricted range of motion can occur if post-operative rehabilitation is delayed or too cautious. Conversely, returning to activity too soon can risk stretching or tearing the repair. Other potential risks include blood clots, shoulder pain, and anaesthetic-related complications, though these are rare. In a small number of patients, particularly younger athletes or those involved in contact sports, re-dislocation may occur. Occasionally, hardware such as anchors can cause irritation or require removal. Fortunately, with modern arthroscopic techniques and careful patient selection, the overall complication rate is low. Following surgical advice, keeping the wounds clean, wearing the sling as prescribed, and attending physiotherapy appointments all help minimise risk and promote successful outcomes. Most patients recover safely and regain stable, functional shoulders.
How long does the repair last?
A Bankart repair, whether performed arthroscopically or through an open technique, is designed to provide long-term shoulder stability. In most cases, the results are durable for many years, especially when the surgery is performed for the right indication and followed by a structured rehabilitation program. The repaired tissue — typically the labrum and capsule — heals back to the glenoid rim, restoring the anatomy that maintains shoulder stability. Clinical studies have shown that approximately 85–95% of patients achieve long-term stability and do not experience further dislocations. However, the longevity of the repair can depend on several factors such as patient age, activity level, tissue quality, and adherence to post-operative restrictions. For instance, younger athletes involved in contact sports like rugby or AFL are at a slightly higher risk of re-injury, even after a successful repair. Degenerative changes, further trauma, or premature return to sport may also compromise the repair over time. Generally, if the shoulder is protected during the healing phase and strengthened appropriately, most patients enjoy a stable shoulder for many years, often for life. Regular physiotherapy and maintaining shoulder strength and flexibility are key to ensuring the repair remains effective in the long term.